What is perimenopause & WTH is happening to me?
Most people are familiar with the idea of menopause, but “perimenopause?” What's the story there? How do we figure out if we're on that journey?
And, why does it even matter?
I’m so glad you’re here, empowering yourself with knowledge on one of the biggest transitions your body will ever go through.
Let’s start by getting clear on some of the terms that a woman will hear as she passes through her 30s, 40s and into her 50s:
Perimenopause = The 6-10 year transition period before menopause. Her hormones fluctuate wildly. Typically starts late 30s into early 40s. “Like puberty in reverse.”
Menopause = The day she has had no period for 12 months, at an appropriate age. (Average age in North America = 51) This is really a moment in time.
Post-menopause = From month 13 onward, for the rest of her life.
We often lump the whole lot of these phases under 'menopause,' which muddies the waters and makes things confusing.
Perimenopause is the runway leading up to menopause, and though it usually starts in the late 30s/early 40s, it can start as young as 30 or as late as the late 50s! The timing of when you go into peri/menopause depends on a lot of variables, including your health status and genetics.
Perimenopause often throws women for a loop, largely because we're left in the dark about it and because it tends to kick off earlier than most women expect. (And it's not just women left out of the loop; it's pretty much everyone, doctors included! See my previous post on why that is.)
So what happens in perimenopause?
Simple answer: your hormones go on a bit of a rollercoaster ride.
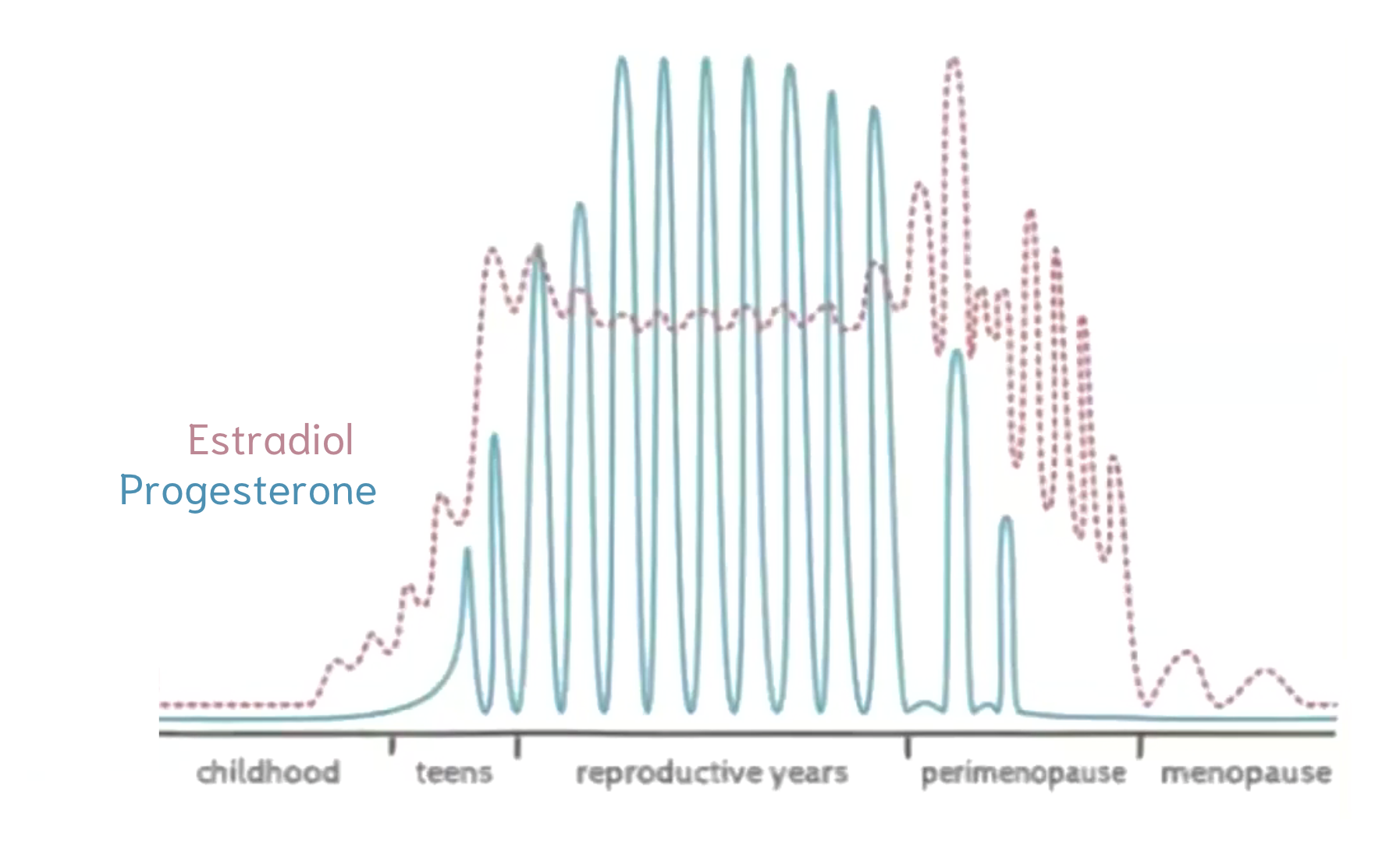
Namely, your levels of progesterone start to decline.
Why does this matter? Because progesterone has tremendous effects on your brain and mood - it’s a calming hormone that helps you sleep, levels out your mood and staves off anxiety, among other things.
Normally, your progesterone surges in the second half of your cycle, which helps balance out estrogen.
Check it out:
When progesterone levels fall relative to estrogen, women can become “estrogen dominant.” This can come with all kinds of symptoms (like weight gain, headaches, decreased sex drive, fatigue, depression, anxiety, etc)…but it doesn’t have to, and this is the point of why I’m creating all this content. The suffering is optional.
And, I should point out, this isn’t the case for all women: every body is different and symptoms vary widely. Some women have zero symptoms and sail through this part of life barely noticing anything is different. Very stoked for them, and I can already say I wish that was me.
Anyhoo.
Through the years, as you progress deeper into perimenopause, the progesterone roller coaster eventually slows to a trickle and estrogen becomes the dominant player every month…until it too eventually slows to a trickle. Then, you’ve found menopause.
As a result of this initial reduction in progesterone, ~75% of women encounter a mix of VERY COMMON YET UNEXPECTED physical and emotional symptoms that catch them off-guard.
As I just wrote about in this article, most women are under the impression that hot flashes are the major symptom to watch for, but actually, there are more common symptoms to be aware of. The most common symptoms are:
fatigue
sleep issues
memory loss/forgetfulness
anxiety
joint pain
lack of concentration
lack of focus
hot flashes
loss of or low libido
Mood changes
Dry skin
Lack of patience
…And these are just a few of them! As I mentioned in the article linked above (and here), the symptoms vary a LOT from woman to woman. In fact, a very recent white paper identified at least 103 perimenopausal symptoms! The authors are still adding to the list. Unfortunately, most doctors are not aware that most of these symptoms are related to perimenopause.
And, since many of these symptoms appear WELL before your periods become irregular, many women (and their doctors) don’t make the link to menopause.
When you look at the symptoms, it's easy to see how they might be mistaken for other health issues, such as thyroid disorders, depression, and anxiety - over 50% are psychological! They could easily brushed off as simply stress-related, especially considering the general pace of life for most women in their early 40s – juggling work, kids, aging parents, and all sorts of demands.
And when mood swings or thinning patience become part of your daily routine, it's not unusual to wonder if you're losing your mind.
The worry deepens with brain fog or memory lapses, stirring fears of more serious conditions like early-onset Alzheimer's.
I remember having my first (and so far, only) panic attack when I was 41, which shocked the hell of out me. Knowing it was probably linked to perimenopause would have been very reassuring.
As I mentioned, women aren't alone in being caught off-guard by perimenopause; many doctors are too, given the “profoundly inadequate” training they receive on the topic, as described in a recent scientific review (2022). It's not uncommon for women to seek medical advice for feeling "off" or experiencing anxiety or depression, only to be prescribed SSRIs without consideration for the fact that they are in perimenopause.
Along the same lines, visiting your doctor during this time will probably result in being dismissed without proper treatment or guidance, as I’ve written about here. I’m about to publish another article on how to support your transition with the information you need to succeed when it comes to leveraging your doctor’s help.
How I know I’m in perimenopause?
One of the most common questions I get is: “How do I know?”
Currently, there's no definitive test for perimenopause.
The earliest signs are usually:
1. Changes in your cycle:
- Shorter cycles: from 28 to ~25/26 days
- Lighter flow
2. Symptoms like the ones listed above, but most commonly, disrupted sleep.
Tracking your cycles is a great first step to understanding where you’re at (although certain contraceptives that affect your cycle can complicate this). There are excellent, free apps like Flo or Clue, which include symptom trackers and insightful resources, like articles relevant to your symptoms or the cycle stage you’re in. I personally love and use Flo all the time.
I also wear an Oura Ring, which I LOVE and personally find to be one of the most useful health-improvement tools. (Shop here.) It allows me to track my body temperature (and ovulation) and track symptoms.
It's equally important to monitor your symptoms to identify patterns, both for your own insight and for informed discussions with your doctor.
Speaking of…This is a key time to reconnect with your healthcare provider and stay on top of wellness checks. For many women, especially after having children, years might pass without a doctor's visit. It's better to have these conversations with your doctor before you're in dire need, as discovering you lack the support you thought you had can be incredibly frustrating – a sentiment echoed by many.
While some sail through this transition smoothly, it's a rocky ride for others. Staying vigilant and prepared for changes is vital. Perimenopause can spotlight any underlying vulnerabilities, physically, emotionally, and mentally, acting as a unique health checkpoint in life. It’s the time to focus on your health and ensure no other issues are being missed.
The Phases of Perimenopause
It’s important to know that your symptoms won’t change steady across each stage: progesterone, the primary sex hormone that drops over the course of perimenopause, doesn’t decline steadily - rather, it’s all over the map! Up and down, varying from month to month and bringing it some degree of monthly unpredicatability. But over the years, it will decline - the path just isn’t linear. And, as mentioned, every woman's experience varies due to factors like genetics, lifestyle, and environment.
That said, it can be helpful to know that there are 4 distinct phases of perimenopause, which are marked by distinct hormonal shifts:
1. Very early perimenopause – regular periods, with subtle signs changes (2-5 years)
2. Early menopause transition – irregular cycles (cycles differ by 7+ days)
3. Late menopause transition – skipped period (60 days with no flow)
4. Late Perimenopause – the last period (the 12-month period before you reach menopause).
This whole transition takes anywhere from 4-10 years. Some stages are wilder than others.
Perimenopause calls for an uptick in self-care: nutrition, exercise, sleep, and education on reducing exposure to environmental toxins that can disrupt hormones. These steps are key to navigating the transition.
So the name of the game is unpredictability, and I hope this information empowers you with knowledge and preparation.
Let’s talk about it
This brief 10,000 foot view on perimenopause touches on the transformative nature of this life phase, akin to a complete rewiring of your body that asks you to be patient and expect the unexpected as you learn what your new body needs.
While our culture has some grasp of hormonal changes during puberty, pregnancy, and postpartum, it lacks awareness and support for this stage of life, and this gap extends to workplaces, social circles, healthcare, and even family understanding.
During a webinar I gave, a participant asked how to talk to her doctor and her family about her symptoms, and I applauded her. This kind of communication is critical: a lot of the distress women feel around perimenopause is that we are trying to manage all of it on our own and we don’t really have anyone we feel we can speak to about it. Managing perimenopause can feel isolating without open dialogue. I sure wish I'd discussed it more with my mom when she was going through it.
There's also a dire need for more clinical education for our healthcare providers so they can provide comprehensive care and support.
In the meantime, we need open conversations, compassion and support.
Exciting times ahead
Yes, perimenopause and menopause topics remain somewhat under wraps culturally.
Yes, the journey begins earlier than many anticipate, presenting health and relational challenges.
But, it's also a phase ripe with opportunity for change and a time in life when women tend to really blossom into our best years.
Much like the life-changing experience of having a child, this transition heralds a new life stage. A significant chunk of our lives – 30-40% – unfolds post-menopause. Perimenopause offers a chance to realign priorities, address health gaps, and rediscover aspects of ourselves sidelined since puberty's hormonal takeover.
This transition isn't something to "fix" but to support, honour and nurture. But that's a conversation for another day.
Stay tuned: more blogs like this coming your way, including “The Hormonal Roller Coaster that is Perimenopause” and “Easing the perimenopause transition: natural ways you can support your hormones.”
If you’ve made it this far, THANK YOU. I appreciate you being here, empowering yourself with wisdom on this topic.
I hope you’ll share this post and/or have more conversations about women’s health with your doctor and with women and men in your life who you care about. Let’s normalize this conversation! <3
If you found this useful, my newsletter is right up your alley.
If you want to go deeper and get my personal help, check out The Better Beyond 40 Formula.